Persistent HPV – what is it and what can you do about it?

HPV that stays in the body for a long time is known as persistent HPV. In this article we answer some of your questions about persistent HPV, including what it is, how long it can persist, how to reduce the risk of HPV-related cancers, and how to clear persistent HPV.
What is persistent HPV?
Persistent HPV is an infection with the human papillomavirus that remains in the body for a long time. Most people who get infected with the HPV virus find their own immune system clears it from their body within about two years. But about one in ten women will not be able to get rid of HPV from their body, and the virus may persist for many years. This is considered a persistent HPV infection.
What causes persistent HPV infection?
We don’t yet know why some people are not able to clear HPV from their body. Scientists are researching the possible reasons why, including studying people’s ability to fight the virus (the immune system), or the way cells in the body that are infected with HPV divide.
Does persistent HPV always cause cancer?
No – having persistent HPV doesn’t mean you will definitely get cancer. But it may increase the risk, in combination with other risk factors. These include smoking, or a weakened immune system.
The best way to reduce your risk of getting HPV in the first place is getting the vaccine to prevent infection, although this doesn’t offer complete protection.
Other ways to reduce your risk of developing an HPV-related cancer include not smoking (or stopping). And remember that going for regular cervical screening tests (smear tests) when you are invited is the best way to pick up any cell changes early. Finding early cell changes means they can be monitored or treated as necessary, before they become cancer.
Which cancers can be caused by HPV?
The main type of cancer caused by HPV infection is cervical cancer. But this is not a common cancer. According to Cancer Research UK (CRUK), cervical cancer is the 14th most common cancer in women in the UK.
HPV can cause some other cancers: of the vagina, vulva, penis, anus and some types of mouth and throat cancer. CRUK reports that these are even rarer than cervical cancer.
How does HPV cause cancer?
There are two types of HPV that are sexually transmitted – low-risk and high-risk. Low-risk types of the virus can cause warts, which have no relation to cancer.
Two of the high-risk types, HPV-16 and HPV-18, cause most HPV-related cancers. If these high-risk types stay in the body for a long time, they can cause changes to the cells and over time the cells can start to divide in an uncontrolled way. This can lead to cancer, in which cells divide and grow out of control, causing tumours.
The UK’s national cervical screening programme is designed to find any signs that cells have changed. These changed cells are called lesions. Low-grade lesions usually clear up on their own.
High-grade lesions may contain precancerous cells, and if left untreated, over about 10-15 years in a person with a healthy immune system these may develop into cancer. With the right monitoring, and treatment, cells that have changed won’t develop into cancer.
How to help clear persistent HPV?
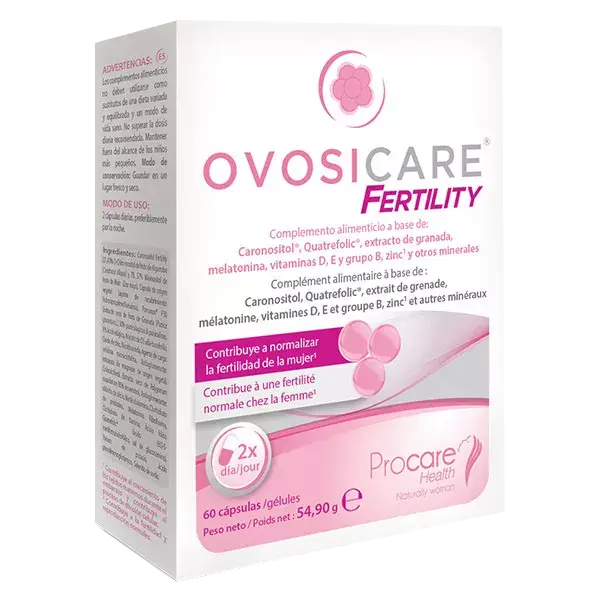
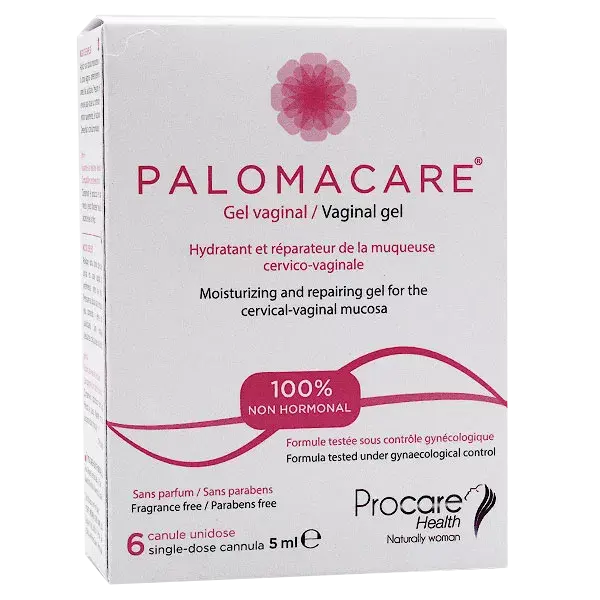
Papilocare® Vaginal Gel is a non-hormonal vaginal gel for the prevention and treatment of HPV-related cervical lesions (cells in the cervix that have changed, also known as abnormal cells). It is based on the natural ingredient Coriolus versicolor, a mushroom traditionally used in Chinese medicine to enhance immunity. Papilocare® Vaginal Gel is applied to and works directly on the cervical-vaginal area, where persistent HPV can sometimes lead to changed, or abnormal, cells.
Is Papilocare® Vaginal Gel proven to work?
In April 2021 the Journal of Lower Genital Tract Disease published the results of the Paloma clinical trial studying how well Papilocare® prevents and treats HPV-related lesions. The study looked at the safety and efficacy of Papilocare® Vaginal Gel.
The study recruited 91 women who had tested positive for HPV and who had changes to the cells of their cervix. The women were randomly split into three groups. Two received treatment with Papilocare® (which varied slightly in duration between the two groups) and a third group had no treatment, but continued on the conventional ‘watchful waiting’ approach.
The results were:
Papilocare® Vaginal Gel was shown to normalise low-grade cervical lesions (changed cells) in 88% of high-risk HPV-positive patients after six months of treatment.
This compared to normalised cervical lesions in 56% of patients in the ‘control’ group, who received no treatment.
Papilocare® Vaginal Gel cleared the virus in 63% of patients who followed the recommended treatment, compared to 40% of the control group
Treatment with Papilocare® Vaginal Gel was safe, and showed good tolerability.
Sources:
https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
https://www.who.int/news-room/fact-sheets/detail/cancer
https://www.hopkinsmedicine.org/health/conditions-and-diseases/human-papillomavirus-hpv/hpv-5-things-all-women-should-know
https://www.cdc.gov/cancer/hpv/basic_info/index.htm
https://www.jostrust.org.uk/information/cervical-cancer/causes-risks?gclid=Cj0KCQiAwJWdBhCYARIsAJc4idA3MK4gI5Mfhu3Mu9b8QlpCV7fAqmkagq-BABAECtTACjb9sGk6XMcaAsVpEALw_wcB
To find out more about persistent HPV visit jostrust.org.uk
Find out more about Papilocare®
HPV that stays in the body for a long time is known as persistent HPV. In this article we answer some of your questions about persistent HPV, including what it is, how long it can persist, how to reduce the risk of HPV-related cancers, and how to clear persistent HPV.
What is persistent HPV?
Persistent HPV is an infection with the human papillomavirus that remains in the body for a long time. Most people who get infected with the HPV virus find their own immune system clears it from their body within about two years. But about one in ten women will not be able to get rid of HPV from their body, and the virus may persist for many years. This is considered a persistent HPV infection.
What causes persistent HPV infection?
We don’t yet know why some people are not able to clear HPV from their body. Scientists are researching the possible reasons why, including studying people’s ability to fight the virus (the immune system), or the way cells in the body that are infected with HPV divide.
Does persistent HPV always cause cancer?
No – having persistent HPV doesn’t mean you will definitely get cancer. But it may increase the risk, in combination with other risk factors. These include smoking, or a weakened immune system.
The best way to reduce your risk of getting HPV in the first place is getting the vaccine to prevent infection, although this doesn’t offer complete protection.
Other ways to reduce your risk of developing an HPV-related cancer include not smoking (or stopping). And remember that going for regular cervical screening tests (smear tests) when you are invited is the best way to pick up any cell changes early. Finding early cell changes means they can be monitored or treated as necessary, before they become cancer.
Which cancers can be caused by HPV?
The main type of cancer caused by HPV infection is cervical cancer. But this is not a common cancer. According to Cancer Research UK (CRUK), cervical cancer is the 14th most common cancer in women in the UK.
HPV can cause some other cancers: of the vagina, vulva, penis, anus and some types of mouth and throat cancer. CRUK reports that these are even rarer than cervical cancer.
How does HPV cause cancer?
There are two types of HPV that are sexually transmitted – low-risk and high-risk. Low-risk types of the virus can cause warts, which have no relation to cancer.
Two of the high-risk types, HPV-16 and HPV-18, cause most HPV-related cancers. If these high-risk types stay in the body for a long time, they can cause changes to the cells and over time the cells can start to divide in an uncontrolled way. This can lead to cancer, in which cells divide and grow out of control, causing tumours.
The UK’s national cervical screening programme is designed to find any signs that cells have changed. These changed cells are called lesions. Low-grade lesions usually clear up on their own.
High-grade lesions may contain precancerous cells, and if left untreated, over about 10-15 years in a person with a healthy immune system these may develop into cancer. With the right monitoring, and treatment, cells that have changed won’t develop into cancer.
How to help clear persistent HPV?
Papilocare® Vaginal Gel is a non-hormonal vaginal gel for the prevention and treatment of HPV-related cervical lesions (cells in the cervix that have changed, also known as abnormal cells). It is based on the natural ingredient Coriolus versicolor, a mushroom traditionally used in Chinese medicine to enhance immunity. Papilocare® Vaginal Gel is applied to and works directly on the cervical-vaginal area, where persistent HPV can sometimes lead to changed, or abnormal, cells.
Is Papilocare® Vaginal Gel proven to work?
In April 2021 the Journal of Lower Genital Tract Disease published the results of the Paloma clinical trial studying how well Papilocare® prevents and treats HPV-related lesions. The study looked at the safety and efficacy of Papilocare® Vaginal Gel.
The study recruited 91 women who had tested positive for HPV and who had changes to the cells of their cervix. The women were randomly split into three groups. Two received treatment with Papilocare® (which varied slightly in duration between the two groups) and a third group had no treatment, but continued on the conventional ‘watchful waiting’ approach.
The results were:
Papilocare® Vaginal Gel was shown to normalise low-grade cervical lesions (changed cells) in 88% of high-risk HPV-positive patients after six months of treatment.
This compared to normalised cervical lesions in 56% of patients in the ‘control’ group, who received no treatment.
Papilocare® Vaginal Gel cleared the virus in 63% of patients who followed the recommended treatment, compared to 40% of the control group
Treatment with Papilocare® Vaginal Gel was safe, and showed good tolerability.
Sources:
https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
https://www.who.int/news-room/fact-sheets/detail/cancer
https://www.hopkinsmedicine.org/health/conditions-and-diseases/human-papillomavirus-hpv/hpv-5-things-all-women-should-know
https://www.cdc.gov/cancer/hpv/basic_info/index.htm
https://www.jostrust.org.uk/information/cervical-cancer/causes-risks?gclid=Cj0KCQiAwJWdBhCYARIsAJc4idA3MK4gI5Mfhu3Mu9b8QlpCV7fAqmkagq-BABAECtTACjb9sGk6XMcaAsVpEALw_wcB
To find out more about persistent HPV visit jostrust.org.uk
Find out more about Papilocare®
Social
Sign up to receive our newsletter and a welcome discount code:
Disclaimer: Information on this website is provided for informational purposes only and not intended as a substitute for the advice provided by your physician or other healthcare professional. You should not use the information on this website for diagnosing or treating a health problem or disease, or prescribing any medication or other treatment. For medical advice, diagnosis and prescription, please consult a healthcare professional. More Information >
Disclaimer: Information on this website is provided for informational purposes only and not intended as a substitute for the advice provided by your physician or other healthcare professional. You should not use the information on this website for diagnosing or treating a health problem or disease, or prescribing any medication or other treatment. For medical advice, diagnosis and prescription, please consult a healthcare professional.
© LivBio Limited 2024 All Rights Reserved.